Calculous prostatitis is a disease in which stony inclusions (or stones) form in the ducts of the prostate gland. It occurs as a consequence of chronic prostatitis. Stones appear from lime salts, phosphates, and prostate secretions. The problem is faced by patients of different age categories: 30 - 40 years old (due to chronic prostatitis), 40 - 60 years old (due to prostate adenoma), after 60 years old (due to the decline of intimate function).
There are exogenous and endogenous types of stones. The composition of exogenous stones can be compared with those found in the urinary tract. They can arise from prostate adenoma and chronic inflammation and are most often found in the distal parts of the prostate. The patient can live with endogenous stones for many years, since they do not cause inconvenience, much less pain. Their cause is congestive prostatitis. Symptoms and treatment of calculous prostatitis require the attention of professionals.
Causes of calculous prostatitis
Chronic calculous prostatitis provokes inflammation and congestion in the prostate gland. Benign prostatic hyperplasia, abstinence from intimate contacts or their irregularity, as well as insufficient physical activity cause improper emptying of the prostate glands. If, in combination with these factors, a genitourinary tract infection is observed, the nature of the prostate secretion gradually undergoes changes.
The disease can also be caused by urethro-prostatic reflux, in which, when urinating from the urethra, a small amount of urine enters the prostate ducts. The salts present in the urine gradually turn into stones. Urethro-prostatic reflux occurs as a consequence of trauma to the urethra, as a result of transurethral resection of the prostate gland, urethral stricture. Urine can enter the prostate after changes that occur during surgical interventions on the genitals, the use of catheters, or the presence of stones in the kidneys or bladder. Stones are mainly urate, oxalate, and phosphate.
Chronic calculous prostatitis can impair reproductive function.
Symptoms of calculous prostatitis
A sign of calculous prostatitis is pain in the lower abdomen, perineum, testicles, sacrum, and scrotum. The diameter and number of stones directly affect the intensity of pain.
Often the pain becomes stronger during and after sexual intercourse, after sitting on something hard, when walking, or vibrations. Aching pain can radiate to the penis and scrotum.
Signals of calculous prostatitis can be the following phenomena:
- frequent urination;
- urinary incontinence;
- the appearance of a small amount of blood in the semen;
- anaphrodisia;
- erectile dysfunction.
A month after the first symptoms appear, the patient may experience a disturbance in his general condition: malaise, decreased performance, depression, irritability, and a slight increase in temperature may be observed.
Diagnosis of calculous prostatitis
When examining a patient, a specialist can only assume that the patient has a disease. Ultrasound of the prostate, magnetic resonance imaging and computed tomography help to detect and confirm the diagnosis of calculous prostatitis.
The next stage is a series of laboratory tests that determine the presence of stones in the prostate gland, as well as the presence and degree of the inflammatory process. The following tests are most often needed:
- general urine test (confirmation is the presence of blood, a large number of leukocytes, protein, epithelial cells);
- general blood test (increased ESR, increased number of leukocytes);
- spermogram (blood is observed, motility and sperm count decreases);
- determination of the level of prostate specific antigen for the purpose of detecting oncological tumors;
- examination of prostate secretions (amyloid bodies, more leukocytes and epithelium are noted).
Later, during instrumental examination, certain signs make it possible to confirm the diagnosis:
- You can find out whether there are stones directly in the prostate by performing an ultrasound;
- A CT scan of the prostate gland will help to find out the location and determine the size;
- With magnetic resonance imaging of the prostate gland, it is also possible to obtain information about the method of formation of stones.
Treatment of calculous prostatitis
Treatment of calculous prostatitis is prescribed and carried out by a specialist; he uses surgery or medication.
The doctor usually chooses a medicinal method in the treatment of calculous prostatitis, provided that the size of the stone is no more than 4 mm. The patient takes anti-inflammatory drugs, antibiotics, and drugs that normalize blood circulation orally and by injection. Herbal medicine is also used. During drug treatment, constant monitoring by the attending physician is important.
Physiotherapy is effective, in many cases facilitating the process of stone passage. For example, magnetic therapy is successfully used, which significantly improves blood microcirculation and has an analgesic and calming effect. Ultrasound therapy is often prescribed; during the procedure, the emitter comes into contact with the skin through a special gel.
Good results are shown by drug electrophoresis, in which the drug is administered through the surface of the skin or mucous membrane using an electric current. In this case, you need to abandon the prostate massage procedure, in contrast to the treatment of chronic prostatitis, in which it is effectively used.
Relatively recently, in combination with medication, the use of low-frequency laser treatment of the prostate has begun. When carrying out such therapy, the stones are gradually crushed and excreted in the urine.
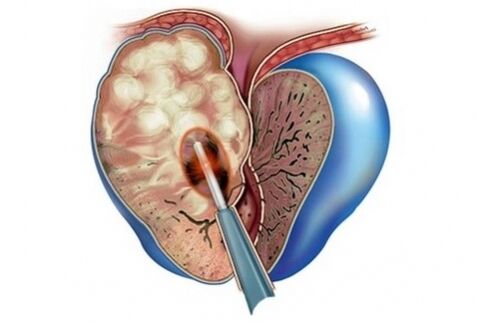
For large stones, drug treatment does not bring results; surgical intervention is undertaken to treat calculous prostatitis. The surgeon removes the stones through an incision in the perineum or suprapubic area.
Calculous prostatitis is often accompanied by BPH. With this option, prostatectomy, adenomectomy, or TUR of the prostate are chosen.
Prostatectomy refers to the removal of the prostate gland, which is performed under general anesthesia. During the operation, the seminal vesicles are also removed. The operation may be abdominal. In this case, the perineum or the anterior abdominal wall is dissected. After removal, sutures are applied.
It is also possible to operate using an endoscope by making several punctures in the abdominal cavity. In this case, rehabilitation is faster.
Adenomectomy is used for large adenomas. Access is through the abdominal cavity. The operation can have a number of complications: bladder fistulas, infection of the genitourinary organs, urinary incontinence, etc.
Transurethral resection of the prostate involves excision of a hyperplastic area of the prostate through the urethra using a resectocystoscope. This operation is less likely to cause side effects, and the recovery period is shorter.
A proper diet is important not only for prevention purposes, but also in the treatment of chronic calculous prostatitis. The diet is prescribed by the attending physician, based on various criteria and factors. Basically, meat, fish and mushroom broths, as well as sauces, spicy dishes, spices, garlic, onions, radishes, are excluded from the daily diet. Limit the consumption of legumes, white cabbage, whole milk, and other foods that promote flatulence. The doctor recommends drinking plenty of fluids.
The sooner the patient consults a specialist, the more favorable the prognosis for the treatment of this disease. If treatment for calculous prostatitis is not carried out, loss of reproductive function, erectile dysfunction, urinary incontinence, sclerosis or abscess of the prostate gland, and injury to tissues located near the stone are possible.
Prevention of calculous prostatitis
Prevention of this disease is relevant for men at any age and includes:
- preventive examinations, lack of self-medication;
- eliminating nicotine from life and reasonable alcohol consumption;
- maintaining an age-appropriate sex life;
- prevention of genital infections;
- physical activity;
- carrying out treatment of infectious diseases.



























